Point of Care Ultrasound for Paramedics and Nurses
POCUSSTUFF
Lung Ultrasound
If you are new to Point of Care Ultrasound scanning the Lungs is a great place to start. By getting comfortable with some basic techniques and training your eye to look for a handful of sonographic signs you will be able to bring to the patient’s bedside a tool that is better than a Chest X Ray at differentiating between several different causes of Acute Respiratory distress.
Lung Ultrasound has demonstrated higher sensitivity and specificity for detecting problems like Pneumothorax, Pulmonary Edema, Pneumonia and Pleural Effusions than what we are able to accomplish with our stethoscope or Chest X-ray.

Bedside Lung Ultrasound in Emergency
BLUE Protocol
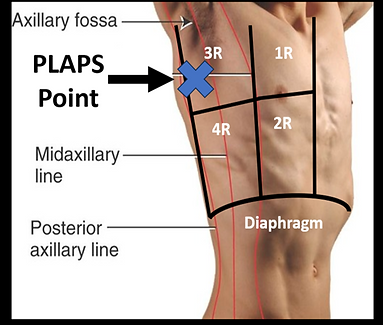
With the use of the Bedside Lung Ultrasound in Emergency (BLUE) protocol we can take a systematic approach to how we evaluate the Lungs using ultrasound. The BLUE protocol involves getting 6 ultrasound lung images, 4 images on the anterior chest at the BLUE points, and 2 images on the Posterior/Lateral Chest at the PLAPS points. As we gather these images we are assessing for the presents or absents of Lung Sliding, A-lines, B-lines, Lung Consolidation, and free fluid within the chest cavity.

Lung Zones
Lung Ultrasound breaks up the chest into 12 Lung zones. Like when we listen to lung sounds the reliability of our ultrasound assessment of the Lungs goes up when we scan in multiple lung zones
Anterior Lung Zones:
-
Zone 1:
-
Sternal boarder to Anterior Axillary Line
-
Clavicle to Nipple Line
-
-
Zone 2:
-
Sternal Boarder to Anterior Axillary Line
-
Nipple Line to Diaphragm
-
Lateral Lung Zones:
-
Zone 3:
-
Anterior Axillary Line to Posterior Axillary Line
-
Axillary Fossa to extended Nipple Line
-
-
Zone 4:
-
Anterior Axillary Line to Posterior Axillary Line
-
Extended Nipple Line to Diaphragm
-
Posterior Lung Zones:
-
Zone 5:
-
Spinal Boarder to Posterior Axillary Line
-
Superior Aspect of the Shoulder to Inferior tip of Scapula
-
-
Zone 6:
-
Spinal Boarder to Posterior Axillary Line
-
Inferior tip of the Scapula to Diaphragm
-


BLUE Points
-
Upper BLUE Points:
-
Midclavicular line, 2nd to 3rd Intercostal Space in Lung Zones 1 Bilaterally
-
-
Lower BLUE Points:
-
Midclavicular line, 4th to 5th Intercostal Space in Lung Zones 2 Bilaterally
-

PLAPS Points
Posterior and/or Lateral Aveolar and/or Pleural Syndrome
The PALPS points lie between the Posterior to Mid Axillary Line in the 4th to 5th intercostal space
Scanning Technique
Probe/Preset:
Linear, Phased Array / Lung, FAST, Cardiac, Pediatric Lung
Body Plane:
Sagittal
Probe Indicator:
Towards Head
Depth:
-
6cm to Evaluate for Lung sliding
-
>16cm for Evaluation of Lung Pathology
Location:
-
Anterior: 2nd to 3rd Intercostal Space, Midclavicular Line
-
Lateral 4th to 5th Intercostal Space, Mid to Posterior Axillary Line
Identify:
-
Lung Sliding
-
Horizontal uniformly repeating A-Line reverberations
-
Vertical B-line "comet-tails" that originate at the pleural line and extend to the deep field of the image.
Notes:
Slide Probe downwards towards the feet evaluating for lung sliding in multiple rib spaces. May also consider scanning along the midaxillary line. A shallow scan will optimize visualization of lung sliding. A deeper scan is required to evaluate for B-lines and other pathology. 2 or less B-lines per rib space is considered normal.


A Shallow Lung Scan with the Probe in a Lung Preset and the Depth set to 6cm is helpful to visualize the Lung Pleural and Sliding
A Deep Lung Scan with the Probe depth now Set to >16cm is need to assess for A-Lines, B-Lines, and Lung Pathology.
A Static Lung scan would be where you are only looking at a single rib space verse a Dynamic Scan moving the probe to look at multiple rib spaces in a single scan.



Strong Return
Weak Return

Strong Return
Angle of Insonation
Angle of Insonation refers to the angle the ultrasound beam relative to a tissue surface. The Ultrasound machine relies on the ultrasound energy it transmits to bounce off a tissue and return to probe in order to produce the on screen image. Any Ultrasound energy that does not return to the probe can not be used to make the images we see.
The closer the angle of insonation is 90* between the probe and the tissue of interest the brighter the image will be. This brightest return represents the most amount of ultrasound energy returning to the probe.
Small adjustment have to be made to improve the angle between the tissue or organ we are trying to image and the probe. This is most apparent in Lung Ultrasound. A-lines and B-lines may be difficult to see if you don't have good angle of insonation between the lung pleura and the probe.

Optimizing Angle of Insonation to better see A-Lines and B-Lines
In order to ensure you have good angle of insonation between the lung tissue and the probe first make sure the pleural line is horizontal on the screen. This will allow for as close to a 90* angle as possible.

Next, with the probe marker pointed towards the head, Fan the probe left and right until you get the brightest image possible. This brightest image means the most amount of ultrasound energy is returning to the probe and should highlight any A or B Lines.
Lung Sliding
The first Step of the BLUE Protocol is to assess for the presents or absents of Lung Sliding. Lung Sliding is a sonographic sign caused by the fully inflated lung sliding against the inside of the chest wall as the patient breaths. Lung Sliding would be absent in cases such as Pneumothorax where the lung has collapsed and no longer touches the inside of the chest wall, or through a pulmonary disease process that has adhered the lung tissue to the chest wall and is no longer mobile.


The presents of Lung Sliding nearly completely rules out the presents of a pneumothorax within the rib space you are imaging having a negative predictive value of 99.2-100% (Blavias 2005, Lichtenstien 2008).

No Lung Sliding
The absents of Lung Sliding alone does not confirm the presents of a pneumothorax. Lung sliding can also be absent if the patient is not breathing, has a right main stem intubation and the left lung is not being ventilated. Disease processes like Pulmonary Fibrosis, ARDS, and large pulmonary consolidations can adhere the lungs to the inside of the chest wall, not allowing lung sliding.

After you have assessed for lung sliding, the next step is to look for A-lines and B-lines and whether or not they are present bilaterally. The presents and distribution of these sonographic signs will help you determine the cause of the patient's respiratory distress.
Lung Ultrasound requires some understanding of image artifacts caused by the ultrasound machine. Two assumptions the ultrasound machine makes is that an ultrasound pulse will be transmitted and return to the probe at a uniform speed of 1540m/s, the speed of sound through soft tissue, and that for each pulse of sound there will be only one return signal without additional reverberation. The ultrasound machine uses this speed in its calculation to determine depth or distance from the probe (Distance = Rate (1540m/s) x Time). Any changes to the transmission speed, or extra echos from a single target causing delayed (increased time) return signals back to the probe, violates those assumptions and will impact how the ultrasound machine forms the on-screen image.
Lung Ultrasound violates these assumptions when the ultrasound pulse encounters air (330m/s) slowing and scattering the beam effecting the RATE portion of the calculation. The Pleura is also highly reflective to ultrasound energy and is known as a specular reflector. By being highly reflective this causes reverberation, meaning that a single pulse of ultrasound energy will hit a target, and reflect off multiple structures before returning to the probe. This increased travel time will impact the TIME portion of the equation and these later returns will be plotted as deeper structures on the screen.
A-Lines
Reverberation Artifact

A-lines are uniformly repeating horizontal lines plotted deeper to the pleural line. These are caused when a single pulse of ultrasound energy reflects off the pleural line, then returns to the probe and then makes multiple trips back and forth between the probe and pleural line. Each time that pulse of ultrasound energy returns to the probe the ultrasound machine will plot that as an additional return.
A-lines will be present in the normal lung with lung sliding when it is aerated, and when lung sliding is absent in the presents of Pneumothorax and there is air within the chest cavity.

B-Lines
Ring Down Artifact

B-lines are 1) Vertical hyperechoic structures 2) Start from and move with the Pleural line 3) Extend to bottom of the ultrasound image 4) Eliminate any A-lines they cross. Two or less B-lines per rib space is considered normal. 3 or more is abnormal and indicates the presents of excess fluid within the lung tissue.
B-Lines are caused when a ultrasound pulse encounters a collection of fluid surrounded by a ring of air or gas bubbles. This Air/Fluid combination slows and scatters the beam causing this vertical "comet tail" appearance.

A Profile


A Profile would be where you see Lung Sliding and A-lines at Each of the Blue points or along your dynamic scan following the midclavicular line. This pattern rules out the presents of a pneumothorax in the lung zone or rib space scanned. It also decreases the likelihood of Pulmonary Edema, and Pneumonia as causes of the patient's respiratory distress. However, to determine the underlying cause of the respiratory distress additional imaging will be required.
The Next step the BLUE Protocol asks is to do a vascular scan and assess for the presents of a DVT. The combination of a physical examination with risk factors for DVT formation, and a Vascular scan positive for an embolism increases the probability of Pulmonary Embolism.
If No DVT is seen the next step is to scan the patient Posterior Lateral side in Lung Zones 3 and 4 bilaterally at the PLAPS (Posterior and/or Lateral Alveolar and/or Pleural Syndrome) points.


Negative PLAPS
The PLAPS Points would be negative if you continue to see Lung Sliding and A-lines at these locations. This would represent sonographically normal lungs and would make it more likely the respiratory distress is be caused be COPD or Asthma.

Positive PLAPS

The PLAPS Points would be positive if you find evidence of Lung Consolidation. This would be where the normally aerated lungs have become so filled with fluids and exudate from a pulmonary disease such as pneumonia that it begins to look more like a solid organ like the liver. This process is called Hepatization.
Lung Consolidation

Pleural Effusion
These points would also be positive if you found evidence of free fluid within the chest cavity. Free Fluid can be the result of Blood such as a Hemothorax in trauma or due to a Pleural Effusion.
Pleural Effusion can be caused by a variety of reasons such as, pulmonary disease processes like Pneumonia, Heart Failure, Cancer, and Liver Cirrhosis.
If the Pleural Effusion is large enough this may be the cause or a contributing factor to the patient's respiratory distress.
B Profile


B Profile would be where you see lung sliding and find Pathological B-lines (3 or mor per rib space) at each of the BLUE Points Bilaterally. This pattern is 97% sensitive 95% specific for Pulmonary Edema (Lichtenstien 2008). The Bilateral B-lines tells use there is disease process that is affecting both lungs causing there to be excess fluid. Pulmonary Edema is common in Heart Failure, but can also be seen in Hypertensive Crisis, Kidney Failure, and Transfusion Reactions. Because in this case there is lung sliding with the B-Lines the Profile rules out the present of Pneumothorax.
A/B Profile

A/B profile is where you see A Profile (Lung sliding with A-lines) in one Lung and B Profile (Lung Sliding with B-lines) in the other lung. The pattern suggests an unilateral exudative process that has increased the fluid content in the lung on the side of the B-Lines. This would indicate the likely presents of a pneumonia on that side.

A' Profile

A' (A Prime) Profile is when you see A Lines without Lung Sliding. The absents of lung sliding alone does not confirm the presents of a pneumothorax. In order to confirm a pneumothorax you must be able to find and identify the lung point. Lung point is the point where a section of partially inflated lung is touching the inside of the chest wall allowing lung sliding to be seen. A through scan of the chest could be required in order to find the lung point.



Lung Point can be absent when a pneumothorax is present when the lung is completely collapsed, and no portion of lung touches the inside of the chest wall being able to cause lung sliding. In these case additional image will be required to determine the cause of the patient's respiratory distress.

Lung Pulse is when you see cardiac pulsations being referred through the lung tissue. This is a normal finding and helps rule out the presents of a pneumothorax in the rib space you are scanning. Lung Pulse and lung point can be confused with each other. To help differentiate between the two consider where you are scanning. You are more likely to see lung pulse on the left chest due to the proximity of the heart. Also lung pulse will mirror the patient's heart rate vs their respiratory rate.
B' Profile
B' (B Prime) Profile is when lung sliding is absent, and B-lines are present on one side. In this scenario a pulmonary process has produced exudates that have adhered the lungs to the chest wall. The B-lines will still start from the pleural line, extend to the deep field, and eliminate any A-lines they cross. The difference here is that because the lung tissue is not mobile, the B-lines will not move with the patient's respirations. This pattern make it likely that the patient has a pneumonia on that side.

**I don't currently have a good example image of B' Profile. If you do please share it with me and the community!**
C Profile

C Profile or Consolidation profile occurs when a pulmonary disease process has produced so much fluid and exudates that the normally aerated lungs begin to take on the appearance of a solid organ this is known as Hepatization. Where the lungs look like the Liver would under ultrasound. This profile would indicate the presents of a Pneumonia.